- What is patient intake?
- Why patient intake efficiency matters
- Patient intake methods, explained
- How to improve the patient intake process
- What to look for in patient intake software
- What challenges does digital patient intake solve?
- What workflows does digital patient intake support?
- Digital patient intake myths, busted
- Conclusion
What is patient intake?

Patient intake is the process through which healthcare organizations collect demographic, social and clinical data, consent forms, insurance, payments and other key pieces of information from new and returning patients prior to their visit.
Patient intake encompasses a wide range of tasks—everything from capturing patients’ addresses, phone numbers and email addresses; collecting medical and social history; verifying eligibility and benefits; collecting copays and balances at the time of service; gathering patient-reported outcomes data; offering patients the option to leave a card on file or set up a payment plan; collecting signed consent forms and more.
Why patient intake efficiency matters
The patient intake process plays a critical role in the operational, financial and clinical success of medical practices and health systems. For instance, an efficient, streamlined intake process means faster throughput and shorter wait times. Consistently collecting at the time of service means less bad debt and increased profitability. And gathering clinical data during intake means providers are better able to care for their patients and meet their quality-improvement goals.
Patient intake also offers opportunities to engage with patients at a range of different points in their care journey and to provide a convenient, high-quality experience. That’s especially important because the intake process is often patients’ first interaction with a healthcare organization, and it sets the tone for their encounter.

But according to the research and insights firm KLAS, the patient intake process in many healthcare organizations is plagued by manual, time-consuming tasks, redundant processes and a lack of customization.
In a report entitled, “Patient Intake Management 2018: Solutions for a More Efficient Practice,” KLAS wrote, “Many outpatient facilities still require patients to fill out paperwork at each visit, and the paperwork is often the same from patient to patient, regardless of gender, age, or reason for visiting the doctor. Clinic employees must then manually enter patients’ responses into clinical and practice management systems. The entire process takes up time that both patients and clinic employees could better spend elsewhere.”
Patient intake methods, explained
For decades, patient intake was a static process across most organization types. It’s what we now think of as “traditional” patient intake: A patient calls to schedule a visit, fills out paperwork when they arrive and receives a mailed invoice for their outstanding balance after the time of service.
But technology has revolutionized most industries, healthcare included. The emergence of digital patient intake software has equipped health systems, hospitals, multispecialty groups and even private practices with more innovative ways to engage patients throughout their patient intake journey. This democratization of patient intake gives healthcare decision-makers—armed with cutting-edge tools and a surplus of choice—the power to fine-tune the patient intake process to meet their organization’s unique needs and optimize inefficient workflows.
So, which patient intake method is best for your organization? If you have an abundance of staff and resources, a traditional patient intake process may suffice. If the healthcare staffing crisis and growing reimbursement challenges are hurting your efficiency and profitability, it may be time to explore a digital patient intake solution instead. And if you’re still on the fence, it’s important to weigh your options—and compare them to your organization’s existing patient intake strategy—before choosing the best path forward.
Pros of traditional patient intake
Traditional patient intake is entirely manual, which can be cumbersome and inefficient. But it also means that staff don’t have to learn any new tools or technologies to perform their jobs.
For veteran administrators and clinicians who’ve spent many years in healthcare, traditional patient intake provides comfortable familiarity. It may be repetitive, but it works: Experienced staffers likely know which forms patients need to sign for common appointment types, and they aren’t afraid of asking for payment at the time of service.
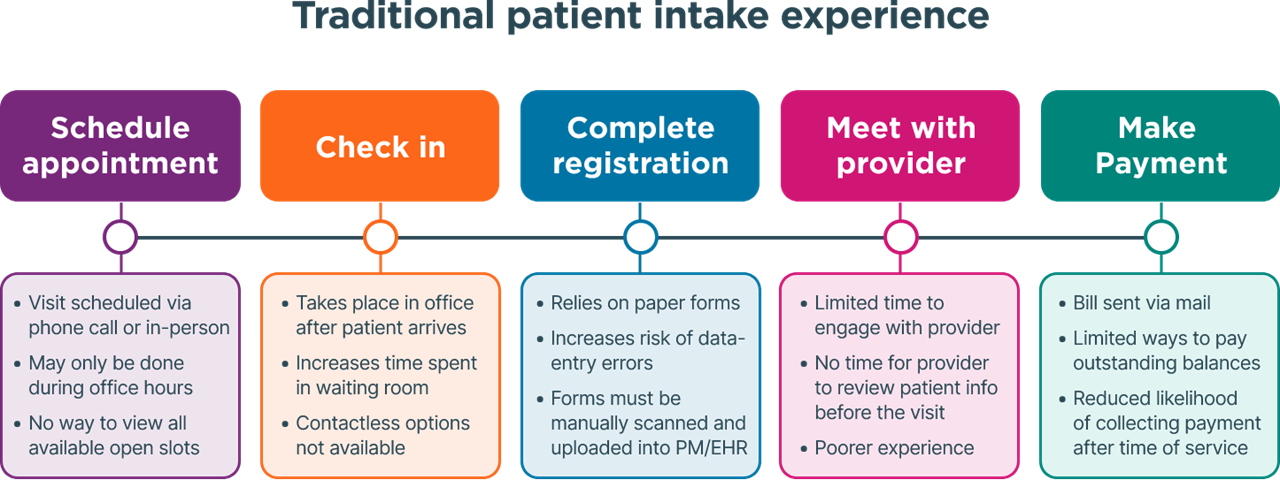
In addition, organizations that use traditional patient intake often rely on fewer third-party vendors, since repetitive administrative and data-entry tasks are handled by staff, rather than supplemented with automation.
Cons of traditional patient intake
Staff burnout has reached critical mass in the healthcare industry, and traditional patient intake is a primary culprit. Among clinicians who are considering switching careers, 89% cite burnout as a key reason why. Nearly 6 in 10 don’t believe their teams are adequately staffed, and 40% feel they lack the resources they need to operate at their full potential.
Traditional patient intake exacerbates those challenges by burdening staff with time-consuming tasks that could otherwise be automated. Some of them, like manual data entry, contribute to serious issues on the backend—like duplicate or mismatched patient records—that can lead to privacy risks, claims denials and reporting errors.

In addition, traditional patient intake leads to a subpar patient experience. Research shows that patients want to use technology to manage their care—and when they don’t have the ability to do so, it hurts their satisfaction and may prompt them to switch providers. Long wait times, low appointment-conversion rates and negative online reviews are often symptoms of a traditional patient intake process. The only way to cure them is by implementing the digital tools that patients of all ages expect.
Pros of digital patient intake
The healthcare industry still has among the highest number of job openings compared to other sectors, according to a March 2023 report from the U.S. Chamber of Commerce. And when front-office team members are in short supply, administrative tasks take longer to complete. The consequences? More bottlenecks at registration, lengthy wait times for appointments and delayed follow-ups—all of which hurt the patient experience.
Digital patient intake automates manual, repetitive tasks so staff have time to give patients the attention they deserve. By streamlining registration, scheduling, payments and consents, digital patient intake helps healthcare organizations alleviate staffing challenges and boost efficiency without adding more employees.
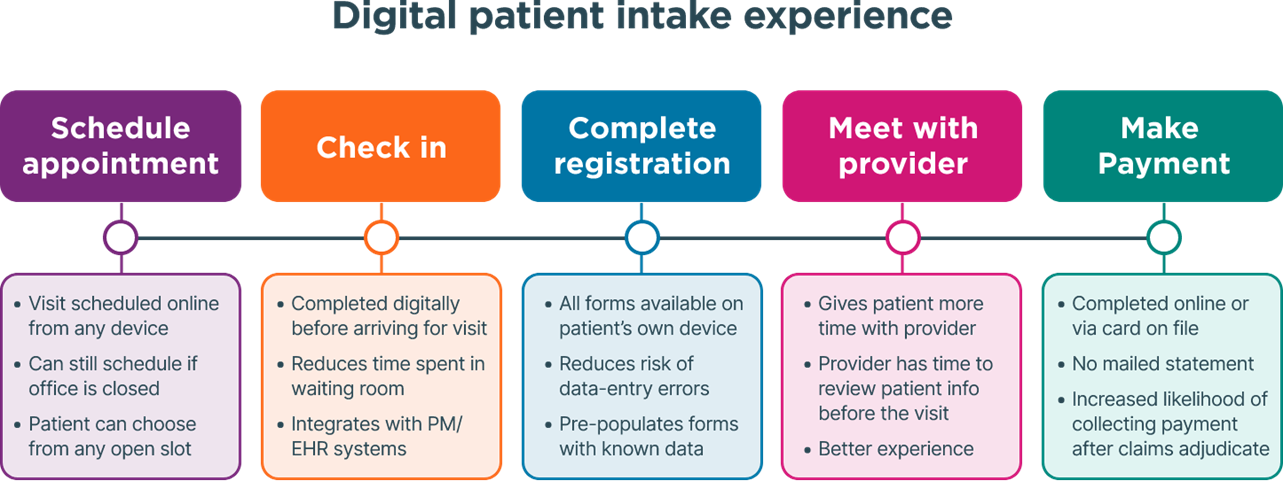
In addition to time savings, digital patient intake helps healthcare organizations align with patients’ ever-evolving needs and preferences. Across age groups, patients enjoy using technology to communicate with their providers. They also prefer to see doctors who offer online check-in, and they would use digital tools to schedule and reschedule their appointments if given the option, Phreesia research shows. In fact, many patients consider digital capabilities to be a “must-have” when choosing a doctor—and they may opt to switch providers entirely if their technology expectations are unmet.
Why digital patient intake is growing in popularity
The rise of consumerism has given patients more ownership of their care than ever before. As patients shoulder an ever-growing share of their healthcare costs, they’re increasingly seeking out convenience, flexibility and other service-oriented features that they’re used to encountering in other industries, such as retail, banking and travel.
For staff, a digital patient intake solution reduces the manual tasks they’re required to perform, such as collecting patient balances, scanning forms or calling insurers to verify patients’ coverage. Automating those processes gives them room to focus on higher-value responsibilities, including their interactions with patients. Alleviating some of that workload and freeing up staff to focus on patients decreases burnout, boosts engagement and increases retention. And not surprisingly, the experience of staff is directly linked to the experience of patients.
Consider this: A study in the Journal of Medical Practice Management found that 96% of patients’ negative online reviews of medical practices were related to service issues, such as poor staff communication or long wait times. Addressing the time-consuming processes that take staff time and attention away from patients can go a long way toward addressing that problem and ensuring that patients are engaged and satisfied.
For clinicians, automating the patient intake process can also result in shorter wait times and fewer bottlenecks, fewer redundant data-entry tasks, and more comprehensive, actionable clinical data during the encounter.
How to improve the patient intake process
In its 2018 report, KLAS emphasized the benefits of automating the patient intake process.
“Patient intake management solutions have the potential to eliminate much of this duplicative and unnecessary work, offering integration with clinical and financial solutions and fluid question sets that can be customized to individual patients,” KLAS said in the report. “In addition to increasing efficiency, improving data capture, and boosting patient satisfaction, these solutions can also have direct financial impacts.”
Indeed, automating the patient intake process can go a long way in helping healthcare organizations streamline repetitive tasks—and even increase revenue. But what specifically should healthcare decision-makers do to implement the right digital patient intake tools for their organization?
Consider the following strategies to build a robust, user-friendly patient intake experience that accommodates the needs and demands of patients and staff alike.
Let patients check in digitally
Digital check-in isn’t a new concept. Most consumers already use their personal devices to check in for flights, hotels, dinner reservations and more. Why not give patients the same convenience for their medical appointments, too?
Online check-in allows patients to complete pre-visit tasks from anywhere—at home, on the go or in your office. Healthcare organizations can send patients a check-in link via text message or email before their visit, which means they don’t have to download an app or create a username and password to check in. Many digital check-in solutions integrate with leading PM/EHR systems, which means returning patients’ information will be pre-populated so they don’t have to manually enter it again. And because digital check-in can be completed before the visit, patients can spend less time in the waiting room when they arrive.
It’s worth noting, of course, that not all patients will check in before reaching the office. Some patients may not own a smartphone, or they may simply forget to click the link to check in. That’s why healthcare organizations should invest in patient intake solutions that support in-office tools for digital check-in—such as patient intake tablets and kiosks—so patients can review and update their information in the waiting room without wasting time on paperwork.
Offer online scheduling
Answering phone calls from patients can be time-consuming—and administrative staff usually shoulder the burden. According to research from Accenture, healthcare staff typically spend more than eight minutes on the phone with each patient who calls to schedule an appointment. That time adds up—especially for organizations with limited resources.
The solution? Empower patients to schedule or request their own appointments instead.
Rather than hiring more people to answer phones, provider organizations can offer patients online scheduling tools that give them more ownership of their care. Self-scheduling typically takes less than a minute and allows patients to book appointments from their own device without calling their provider’s office. Alternatively, healthcare organizations can offer patients online appointment requests to reduce incoming calls, alleviate front-office burnout and give staff more time to focus on delivering the best-possible patient experience.
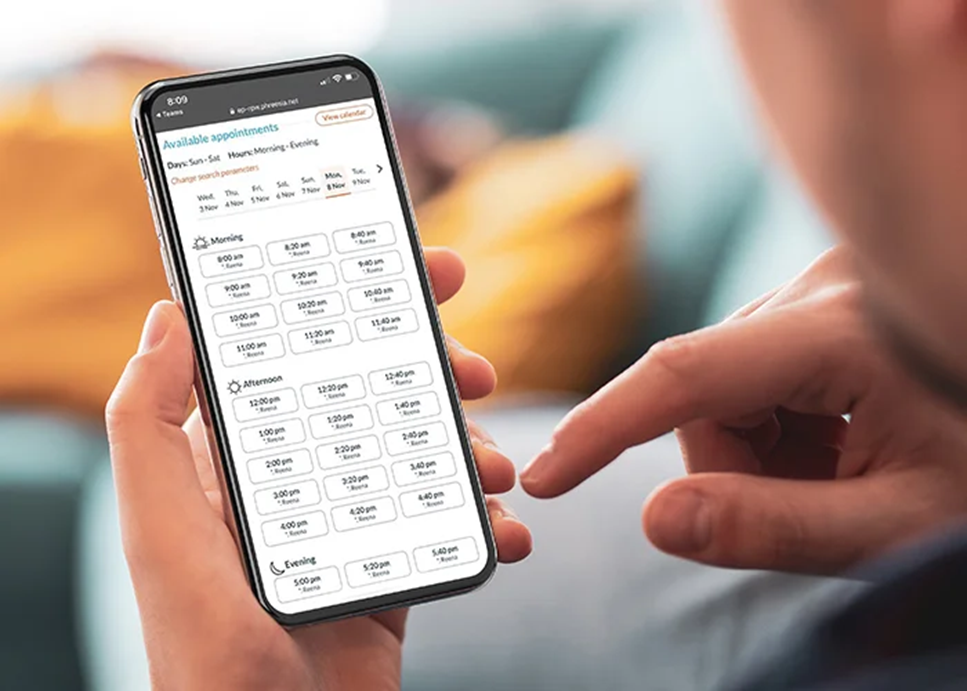
Online scheduling also aligns with healthcare consumers’ evolving preferences, considering that 93% of patients say they want more digital conveniences to manage their healthcare. By delivering the tech-enabled experience patients prefer and expect, providers can increase efficiency, boost satisfaction and stay competitive—even in the face of formidable staffing headwinds.
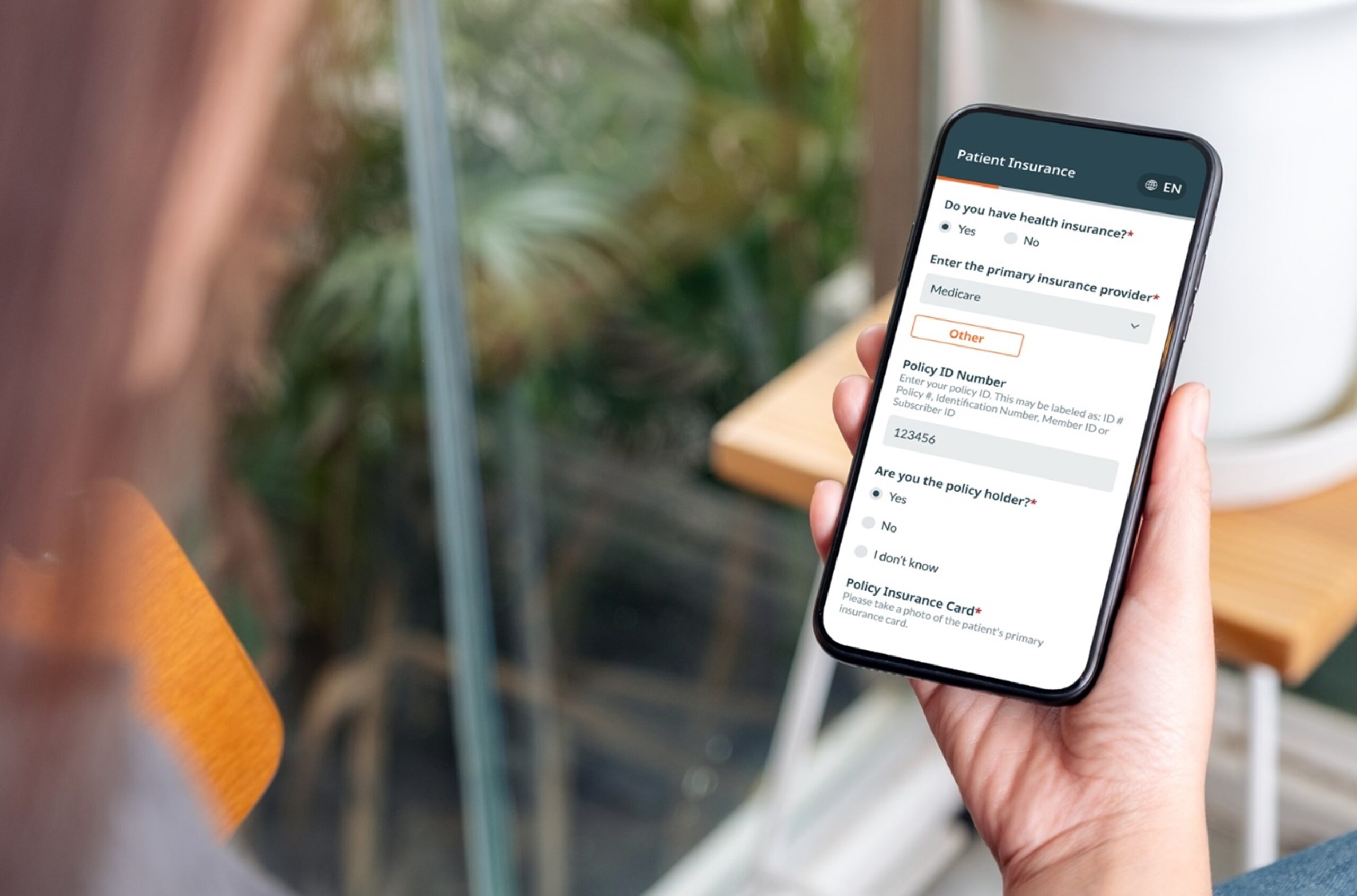
Automatically verify insurance
Verifying patients’ eligibility and benefits is crucial for ensuring timely reimbursement. But manual verification is also cumbersome and error-prone, which can undermine healthcare organizations’ efficiency and increase the likelihood of denied claims, depleting the cashflow that healthcare organizations need to run their day-to-day operations.
That’s why healthcare organizations should look for patient intake tools that automatically check patients’ eligibility and benefits before they arrive for a visit. Here are a few key benefits of automating E&B checks:
- More approved claims: Research shows that more than half of claims denials are the result of mistakes made on the front end. Automated E&B checks minimize that risk, and they allow staff to easily edit and resubmit 270/271 Transaction Sets if errors do occur.
- Significant time savings: Research shows that medical providers could save 21 minutes per transaction by electronically verifying E&B. Automation also helps staff verify patients’ coverage for various service type codes and allows them to easily flag patients’ primary, secondary and specialty insurance during patient intake.
- Lower labor costs: Healthcare organizations spend more than $5 in labor costs each time they manually check patients’ eligibility and benefits—and those costs are likely to increase as wages rise. But if every healthcare organization in the U.S. switched to electronic eligibility checks today, the medical industry could save $9.8 billion per year.
- Better transparency: With automated insurance verification, healthcare organizations can gain immediate visibility into patients’ copay, deductible and out-of-pocket obligations—and staff can educate patients about what they will owe before they enter the exam room.
Collect payments via mobile or tablet
Collecting from patients after their visit has never been easy. Even before the pandemic, more than two-thirds of patients with hospital bills of $500 or less did not pay them in full—and the longer patients go without paying their bill, the less likely they are to ever pay it. Not surprisingly, practice management experts stress the importance of collecting copays and balances at the time of service whenever possible, especially given patients’ growing share of costs.
Consumer-friendly options like online payments, card on file and self-service payment plans help patients better manage their finances as they assume greater responsibility for the costs of their care. Flexible payment options also improve the likelihood that patients will pay their bill in full, which helps healthcare organizations increase collections both at the point of care and after the patient leaves the office.
Indeed, many patient intake solutions give healthcare organizations the ability to collect payments online. But it’s equally important—if not more so—to give patients a variety of options to make a payment, including:
- Credit, debit and FSA/HSA transactions
- Mobile wallets, such as Apple Pay® and Google Pay™
- Cash and check tracking
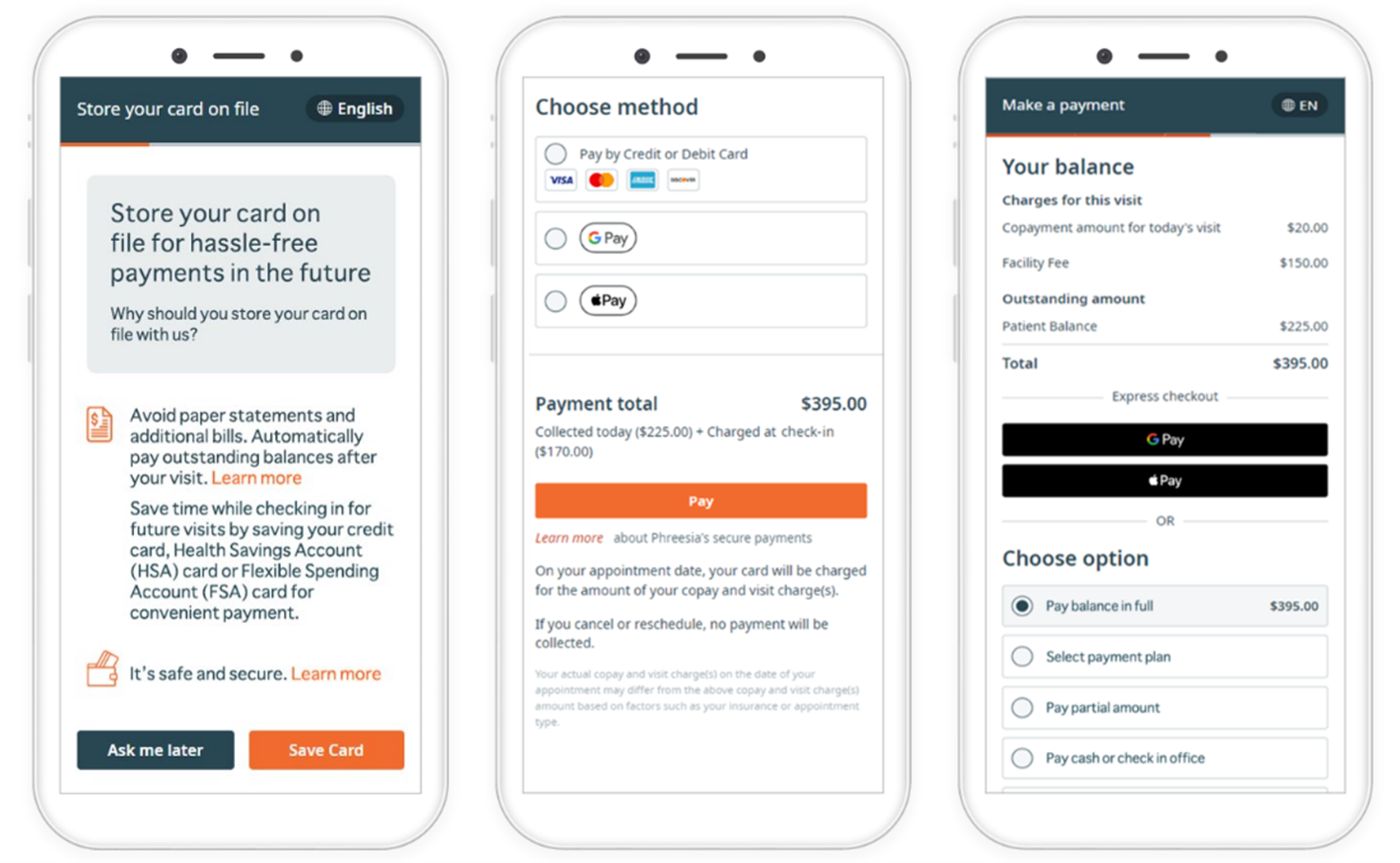
Giving patients multiple ways to pay helps healthcare organizations collect payments faster and more consistently. It can also help reduce hard costs by prompting patients to pay at the time of service and sending digital statements for outstanding balances, minimizing the need to mail paper invoices or pay for postage.
Survey patients about their experience
Are your patients content with the amount of time they spend in the waiting room? Do they understand their doctor’s instructions? Are your front-desk employees courteous and helpful? It’s hard to really know the answers to these questions without consistently asking patients for their direct feedback.
Post-visit patient satisfaction surveys help staff engage patients in a dialogue and send a message that their experience matters. And when patients’ survey responses can be reviewed in real time, healthcare organizations can proactively identify and address issues—and in turn, improve the patient experience.
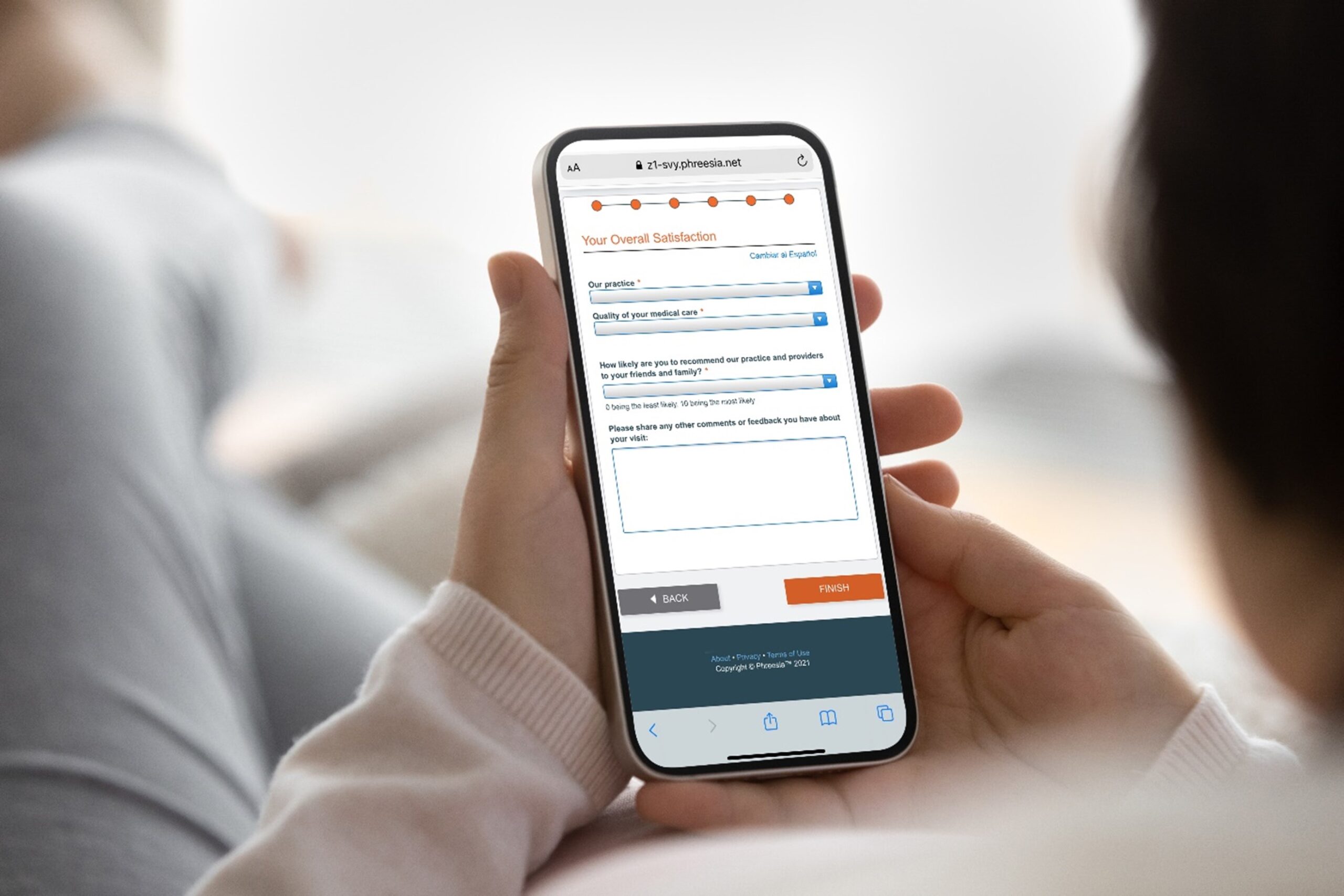
But assessing patients’ feedback isn’t just a “nice-to-have.” It’s also a way to project patients’ likelihood of returning to your organization for care. When patients’ expectations are met, they’re likely to keep coming back. When they aren’t, providers risk losing patients to their competitors— and in some cases, they may face lower reimbursement based upon quality benchmarks.
As healthcare providers become more consumer-driven and patient-centric, patient satisfaction is integral to financial success. By implementing a patient intake solution that surveys patients after the point of care, healthcare organizations can collect accurate, high-quality patient feedback when it matters most.
View analytics and reports
Your healthcare organization, like any other business, is the sum of its parts. To make informed decisions, you need to capture a complete picture of your efficiency and progress—and understand how to improve them.
By implementing a patient intake solution with robust analytics and reporting capabilities, you can more easily identify areas of outperformance and find opportunities for improvement. Better yet, those insights can help you develop actionable steps to reduce overhead, operate more efficiently, stay competitive and keep patients coming back.

Analytics and reporting tools can also help you:
- Discover how new patients are finding you—whether it’s through a phone call, a self-scheduling link, an appointment request form or anything in between.
- Monitor every step of the patient intake process—before, during and after patients’ visits—so your front-office staff doesn’t have to.
- Track staff performance over time, and benchmark your progress toward your organization’s operational, clinical and financial goals.
- Identify missed revenue opportunities, including real-dollar values of unpaid balances, missed copays and denied claims, and develop actionable steps to improve them.
- Bolster preventive care efforts by identifying which patients are due for preventive services, such as annual wellness visits, mammograms or immunizations, and prompting them to schedule a visit.
Measure patient activation
Patient activation—a measure of one’s knowledge, skills and confidence to manage their own health and healthcare—plays a determining role in their healthcare experiences, costs and outcomes. But without a reliable way to assess patient activation, it can be tough for healthcare organizations to determine the appropriate level of support for each patient.
That’s why healthcare decision-makers should look for patient intake tools like the Patient Activation Measure® (PAM®), which provides granular insight into patients’ health-related characteristics—including their attitudes, motivators and behaviors. PAM can be used to:
- Improve segmentation and risk identification by identifying patients with low activation that traditional risk models often miss
- Tailor support to PAM level to establish realistic, achievable goals and action steps through an activation-based approach to coaching and education
- Measure impact to show how patient-support strategies and programs can be understood well in advance of traditional outcome measures
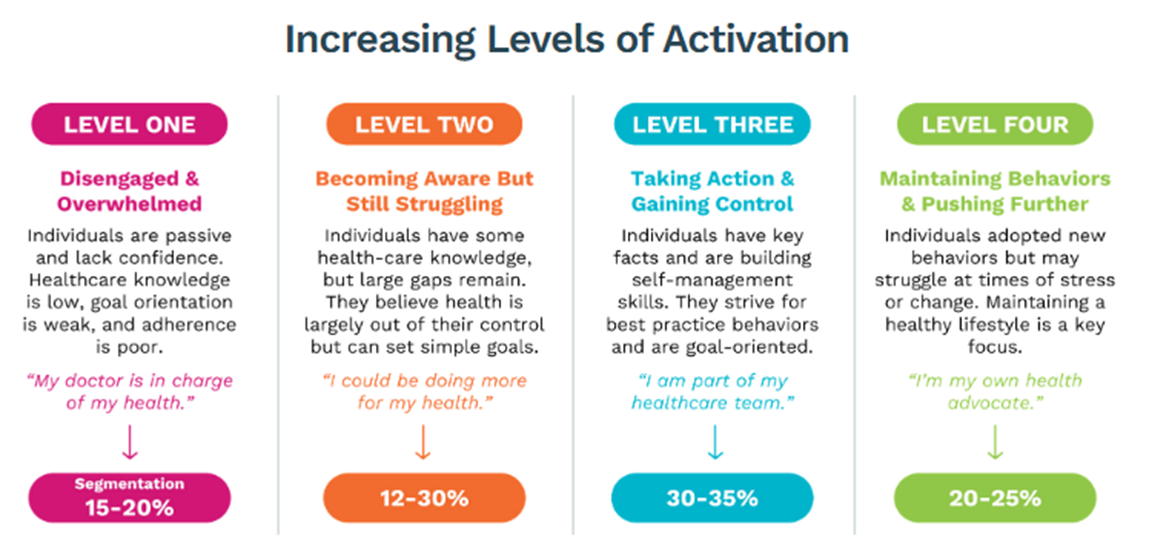
For many healthcare organizations, focusing on patient activation can seem overwhelming amid mounting pressures to improve clinical outcomes, control costs and adapt to new models of care delivery. Yet all these goals are inextricably linked. Helping patients take an active role in their care makes them more engaged, which in turn advances care quality and improves clinical outcomes. Better health outcomes often go hand in hand with lower costs—both of which can boost healthcare organizations’ performance in value-based care arrangements.
By putting patients at the forefront of their care—and equipping them with the ability to self-manage it—providers can better improve the population health of the communities they serve.
What to look for in patient intake software
Not all solutions are created equal. When choosing a patient intake solution and management partner, it’s important to carefully evaluate functionalities, features and capabilities to be sure your organization selects the right solution to meet your needs. Here is a brief list of features to look for that can help guide your search:
| Feature | What it means | How it helps | Phreesia |
|---|---|---|---|
| Bidirectional integration | Allows for seamless data synchronization between the patient intake software and one or more systems, such as a PM, EHR, HIE, data warehouse or data lake. |
| |
| HIPAA compliance | Includes all privacy and security safeguards necessary to comply with the Health Insurance Portability and Accountability Act, which maintains standards for safeguarding protected health information (PHI). |
| |
| Dedicated customer service and support | Ensures clients have a dedicated team from the vendor for implementation, onboarding and training; as well as a dedicated support representative to advise on utilization, troubleshooting and product optimization. |
| |
| Self-service check-in | Gives patients a flexible, user-friendly check-in experience, no matter where they are—at home, on the go or in your office. |
| |
| Online forms and e-consents | Captures patients’ digital signatures and sends required electronic patient intake forms directly to your PM/EHR, without printing or scanning. |
| |
| Insurance verification | Verifies insurance information directly from the patient and conducts automated checks multiple times before the patient’s visit. |
| |
| Appointment requests and self-scheduling | Lets patients self-schedule or request an appointment directly from their own device—anytime, anywhere. |
| |
| Two-way text messaging | Allows providers and staff to communicate with patients by sending individualized text messages that let them connect with you in real time. |
| |
| Appointment reminders | Automatically reminds patients about their upcoming visit via email, text message or voice call, and asks them to confirm, cancel or request to reschedule the appointment. |
| |
| Smart scheduling | Fills open slots on your schedule by sending automated text messages to clinically relevant patients that allow them to instantly claim an earlier appointment. |
| |
| Multiple payment options | Gives patients several ways to pay copays and balances on their own, including mobile wallets, online payments, payment plans and more. |
| |
| Automated post-visit collections | Automatically charges patients’ cards on file to collect outstanding balances after insurance claims are adjudicated—no mailed statements or follow-up calls required. |
| |
| Merchant processing | Handles every aspect of an organization’s payment-processing needs—including funding, chargebacks and fraud monitoring—at a simple rate, with no hidden fees or rate fluctuations. |
| |
| Patient-reported outcome (PRO) collection | Collects and organizes patient-provided information before every visit—and gives providers the information they need to have more meaningful, productive encounters. |
| |
| SDOH screenings | Identifies patients’ social needs privately and securely during intake, enabling providers to deliver more compassionate, holistic care. |
| |
| Post-visit surveys | Enables healthcare organizations to request and assess patients’ feedback after their visit, and allows staff to quickly follow up with patients whose experience was subpar. |
| |
| Intake and outreach campaigns | Lets providers and staff engage with patients before, during and after their visit with tailored email messages that encourage routine care and drive follow-up appointments. |
| |
| Referral management | Automatically transcribes every referral that comes in—whether via fax or online—and lets staff organize, prioritize and standardize them from a single screen. |
| |
| Managed services | Supplements patient intake software by giving organizations a dedicated team of trained administrative and patient support specialists to help manage day-to-day functions. |
| |
| Custom branding and white labeling | Allows a healthcare organization to incorporate its own name, logo and brand guidelines on appointment request forms and patient-facing screens. |
| |
| Workflow management tools | Equips staff with a suite of tools and reports to monitor intake, access patient information and manage registration exceptions—all from one screen. |
| |
| Analytics and reporting | Measures performance and impact for various operational, clinical and financial initiatives, and gives staff greater visibility into patient intake trends and patterns. |
|
What challenges does digital patient intake solve?
It’s well established that traditional patient intake can dampen operational efficiency. But why exactly is digital patient intake a better alternative?
Consider how digital patient intake can help alleviate common challenges and empower staff to accomplish more with less:
Front-office bottlenecks

When administrative staff are swamped with phone calls and paperwork, they don’t have time to engage with patients. The waiting room fills up, and patient flow plummets. Over time, those problems can exacerbate staff burnout and erode patient loyalty.
Automating manual patient intake tasks like check-in, consent management and insurance verification gives your staff more time to focus on patients. By implementing the right digital tools, you’ll operate more efficiently and empower your team to accomplish meaningful work.
Unpredictable schedules

Physicians’ schedules are hectic enough, but they’re even harder to manage when patients don’t show up. Rising no-show rates and appointment cancellations make it tough to predict resourcing needs—and to recoup lost revenue from unexpected open slots.
That’s why healthcare organizations should implement patient intake tools like self-scheduling, smart waitlists and appointment reminders. These solutions make patients more likely to arrive on time for their appointments, which means you’ll expedite care, minimize revenue losses and make the most of your clinicians’ valuable time.
Inaccurate records
Most healthcare leaders view data entry errors as the biggest contributor to duplicate medical records. Reconciling those errors takes time—and failing to fix them leaves healthcare organizations with unreliable information that can impede patient registration. But with a digital patient intake platform, healthcare organizations can collect accurate, high-quality data directly from patients at any time, including before they arrive.
Be sure to choose a solution that integrates with your existing systems. Phreesia’s integrations are managed by a dedicated team skilled in HL7v2, FHIR, proprietary APIs, data extracts and more. In addition, Phreesia collaborates closely with PM and EHR vendors—as well as registration, scheduling, billing and document management systems—to build robust, responsive interfaces that help healthcare organizations save time and have more meaningful patient encounters.
Staff burnout

Is your staff bogged down with repetitive phone calls, manual data entry and other unfulfilling tasks? Do they have the autonomy to creatively solve problems? If not, office morale and employee engagement and retention are bound to suffer.
With a patient intake platform, you can automate repetitive tasks to make sure that your clinicians and front-office personnel have enough time to do the work they love. And if technology isn’t enough to move the needle on burnout, consider alternative strategies—like hosting a daily staff huddle—to discuss problems, brainstorm solutions and amplify your team’s voice.
Inconsistent quality reporting

Value-based care models rely on robust patient data to measure care quality. As such, providers are often tasked with meeting dozens of quality goals—but the reporting requirements for most quality programs can be mind-bogglingly complex.
Fortunately, digital patient intake software automatically captures data for a range of quality measures—from fall-risk assessments to cervical cancer screenings, and many other metrics—during registration. By standardizing the process, you’ll be able to minimize manual data entry, close gaps in care and more easily meet your quality goals.
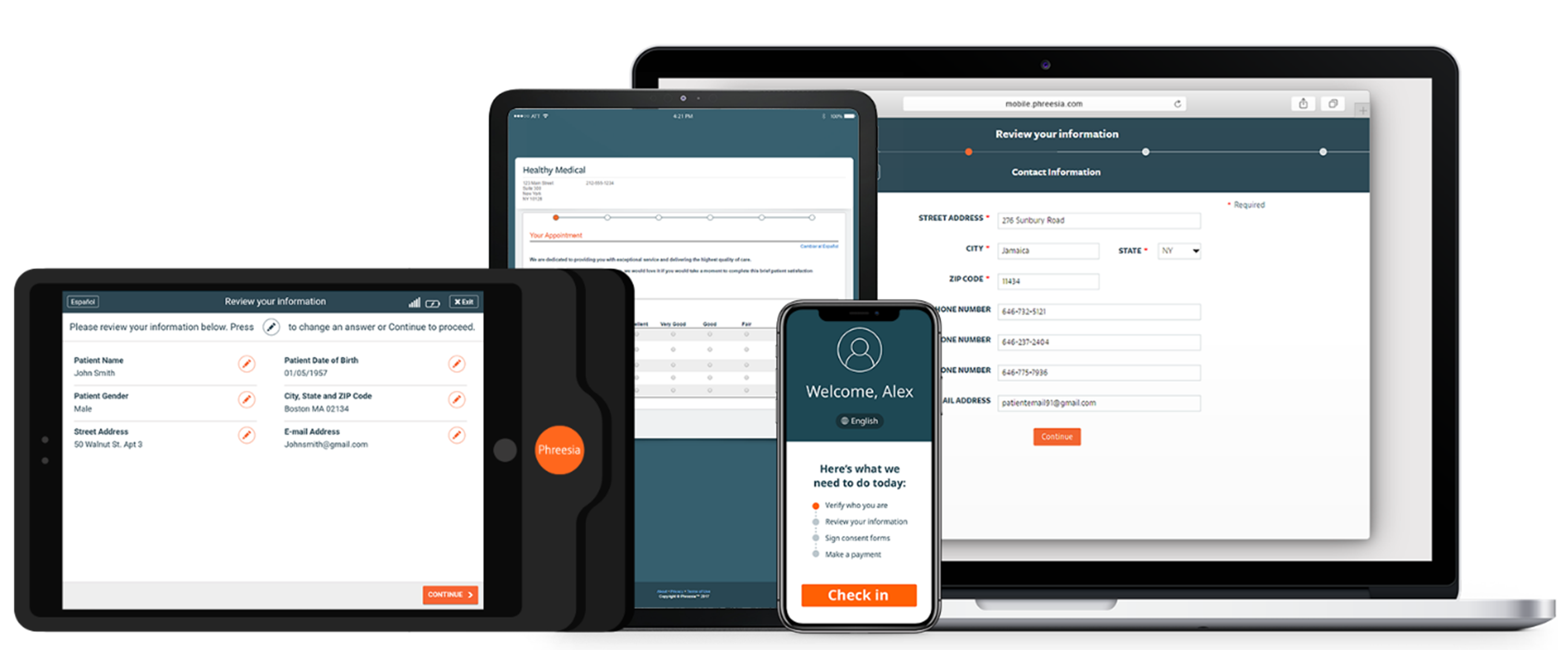
What workflows does digital patient intake support?
Support for multiple modalities is a key differentiator with digital patient intake, allowing patients to engage in their care 24/7. It also enables healthcare organizations to meet the needs of diverse populations—such as varying age ranges or socioeconomic backgrounds—to ensure every patient can self-select the patient intake experience that works best for them.
Mobile patient intake
Mobile patient intake provides a fast, easy way for patients to schedule visits, check in, make payments and more. Patients can manage their intake journey directly from their cell phone, which means they can complete all the pre-visit steps they need to take before reaching the office.
In-office patient intake
When people hear the term “in-office patient intake,” they usually associate it with the old way of doing things—standing in line at the front desk, filling out paper intake forms and receiving a bill in the mail after their visit. But in reality, digital patient intake can be completed in-office, too.

Healthcare organizations can offer patient intake tablets and self-service kiosks that let patients complete digital intake forms when they arrive. It may not reduce their time in the waiting room, but it will meet the needs of patients who don’t own a smartphone. And by choosing an integrated patient intake solution, patients’ responses will automatically sync with the organization’s PM/EHR system, which means staff won’t have to waste time manually entering patients’ responses into their charts.
Patient intake for telehealth
Does your organization offer virtual visits? If so, consider implementing a patient intake solution with built-in telehealth workflows.
Much like mobile intake, patients can complete pre-visit tasks—including signing consents—from their personal device, such as a cell phone or home computer. But with patient intake for telehealth, patients will receive specific instructions and information for the session, as well as a link to enter a virtual waitlist, if applicable. And after the session ends, staff can access and review post-telehealth visit reports.
Digital patient intake myths, busted
Although digital patient intake is growing in popularity, some healthcare organizations are still hesitant to implement it. In many cases, they’re worried that certain patient segments won’t enjoy it—or they feel that it wouldn’t make sense for an organization of their size or specialty.
But many of these misconceptions are based upon unfounded, outdated stereotypes. Here are three of the most common digital patient intake myths:
Myth #1: Older adults won’t understand it
It’s often assumed that older patients don’t understand how to use smartphones or the internet. Worse, they may be averse to technology altogether—and for healthcare leaders looking to modernize, that misconception fuels hesitation. If older patients feel uncomfortable using technology to manage their health, they may struggle to get the care they need.
Here’s the reality: Nearly three-quarters of adults age 70 and older own a smartphone, and 88% of those adults use their smartphones daily. Older adults use technology not only for business and personal reasons, but also to accommodate their evolving needs as they age. Those who are hard of hearing, for example, may prefer communicating via text message rather than over the phone.

In fact, the vast majority of older adults surveyed by Phreesia said they’re willing to use technology for check-in, scheduling, payments and engagement. By leaning into that shift and embracing convenient, easy-to-use patient intake tools, healthcare providers can more quickly respond to older adults’ needs, improve their health outcomes and better engage them in their care.
Myth #2: It doesn’t make sense for smaller organizations
Sure, digital patient intake makes sense for large, complex enterprises with multiple locations and service lines. But there’s no reason for a small private practice or solo provider to implement digital patient intake software—right?
In fact, small practices may reap even more benefit from digital patient intake solutions. The ability for patients to self-schedule alone reduces workloads for staff, enabling small organizations to compete with their larger, better-resourced competitors. Automated reminders for routine wellness exams and screenings also help small practices boost revenue and improve patient outcomes.
Myth #3: It’s less secure than paper-based patient intake
Patients expect their doctors to keep their personal health information safe—but all digital tools are prone to cyberthreats. Understandably, some healthcare organizations worry about technology’s ability to keep their sensitive data secure.
But the truth is, paper-based patient intake is inherently less secure than a digital, HIPAA-compliant patient intake solution. Paper records can easily be accessed by unauthorized individuals—and if patient data falls into the wrong hands, your organization could face legal trouble.
Of course, it’s important to do your homework when assessing patient intake vendors to ensure they prioritize privacy and security at every step of the patient intake journey. So before choosing a vendor, be sure to confirm that they:
- Comply with regulatory standards that keep patients’ health information secure
- Offer PCI-validated solutions that use tokenization and encryption when handling patient payments
- Are certified by comprehensive security compliance frameworks, such as HITRUST and SOC 2
Conclusion
The evolution of patient intake has equipped provider organizations with more modern, convenient ways to engage patients throughout their healthcare journey. The proliferation of digital tools has transformed the patient intake process, empowering staff to operate at peak efficiency and giving patients the ability to self-manage their care more than ever before.
By embracing the shift toward a digital-first patient experience, healthcare organizations everywhere can optimize their workflows, streamline repetitive tasks and deliver more high-quality, compassionate care—no matter their size, specialty, location or patient demographic.
Learn how Phreesia helps healthcare organizations provide a modern, individualized patient intake experience—at scale.





