This is the third in a series of three blog posts about patients’ habits and preferences related to appointments and referrals, covering such topics as patients’ preferred method of scheduling appointments and how often they follow through on referrals. The data featured in this blog series is based on survey responses from nearly 14,000 patients across Phreesia’s network and included in our whitepaper, Appointments and Referrals: Understanding Patients’ Habits and Preferences.
Referring patients to other providers for tests, consultations or additional treatments is one of the most common processes in healthcare. Referrals are an important way to ensure patients get appropriate, coordinated care, and they’re also a key source of new patients and practice revenue for specialists. Referrals are made in nearly 1 in 10 ambulatory appointments in the U.S., resulting in 100 million referrals each year.
Yet as providers know all too well, handing a patient a slip of paper does not necessarily mean that a visit will occur. According to a joint report released earlier this year by the Institute for Healthcare Improvement and the National Patient Safety Foundation, up to 50% of referrals aren’t completed—breakdowns they say can lead to missed or delayed diagnoses and delayed treatment.
 The referrals process is often characterized by multiple calls, long lead times and confusion for patients, and by time-consuming manual tasks and fragmented communication for providers. A growing number of healthcare organizations are trying to align with the trend of consumerism in healthcare by making the referrals process more convenient, flexible and patient-centered. But without good data about patients’ habits and preferences, making changes often involves little more than guesswork.
The referrals process is often characterized by multiple calls, long lead times and confusion for patients, and by time-consuming manual tasks and fragmented communication for providers. A growing number of healthcare organizations are trying to align with the trend of consumerism in healthcare by making the referrals process more convenient, flexible and patient-centered. But without good data about patients’ habits and preferences, making changes often involves little more than guesswork.
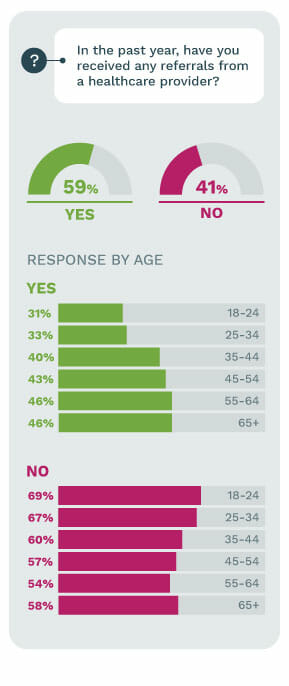
According to Phreesia’s survey of nearly 14,000 patients, 41% said they had received a referral during the past year. Those percentages were higher among older patients, not surprisingly given their higher rates of chronic diseases and higher usage of healthcare services. Among patients ages 18 to 24, only 31% had received a referral in the past year. That percentage jumped to 43% among respondents ages 45 to 54 and to 46% among patients aged 65 and older.
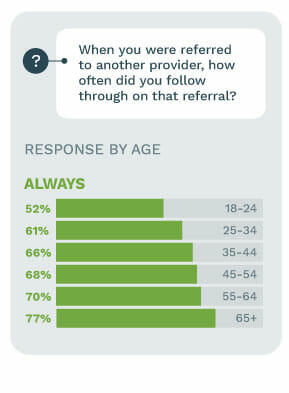
When patients were asked how often they followed through on referrals, 69% said “always,” 18% said “very often,” 9% said “sometimes,” 2.2% said “rarely” and 3% said “never.” But once again, responses depended heavily on patients’ age. Among the youngest patients, ages 18 to 25, the rates for “sometimes” “rarely” and “never” following through on referrals jumped to 15%, 8% and 5%, respectively. Patients 65 and older reported always following through on referrals 77% of the time, with only 1% saying they never follow through.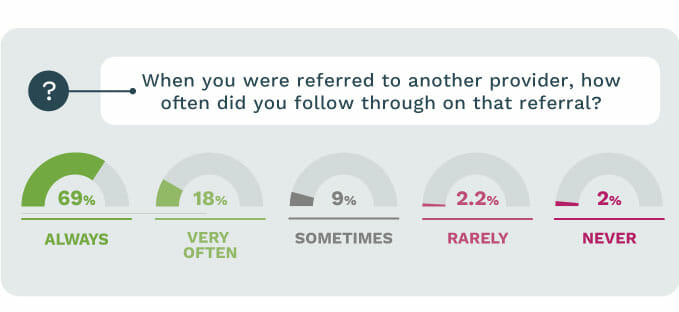
Healthcare organizations need to take these generational differences into account when devising strategies to engage patients and improve their experience—while still avoiding the myth that older adults are resistant to use technology.
Perhaps the most challenging black box related the referrals process is why so many patients don’t follow through on their visits. When surveyed patients were asked that exact question, they cited a mix of factors. Twenty-two percent said they felt better, 14% said they forgot, 14% said they went to a different healthcare provider, 13% said the cost was too high, and 6% said they were confused about what to do.
Once again, age matters. Nearly a quarter of respondents ages 18 to 24 said the primary reason they don’t follow through on referrals is because they forgot, while only 7% of those 65 and older gave that reason. Interestingly, 22% of those over 65 cited going to a different provider as the primary reason why they did not follow through, the highest rate of any age group. Cost concerns also seemed to rise with age, with 15% of adults ages 55 to 64 listing it as their primary reason for not following through. That percentage drops to 6% among respondents over 65, perhaps because those patients have reached the eligibility age for Medicare.
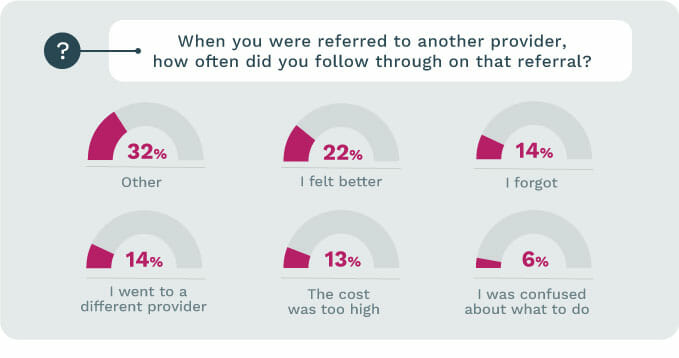 What are the takeaways from this portion of the survey data? Whether a patient receives referrals, whether they follow through on them, and the reasons why they don’t follow through are highly dependent on age. Practices’ efforts to streamline the referrals process and make it more convenient should take into account those generational differences. In addition, clear communication with patients, price transparency, reminders and other improvements can help to address the specific reasons why patients say they don’t follow through.
What are the takeaways from this portion of the survey data? Whether a patient receives referrals, whether they follow through on them, and the reasons why they don’t follow through are highly dependent on age. Practices’ efforts to streamline the referrals process and make it more convenient should take into account those generational differences. In addition, clear communication with patients, price transparency, reminders and other improvements can help to address the specific reasons why patients say they don’t follow through.
Learn more about Phreesia’s Patient Appointment Scheduling Software.





