A TAILORED SOLUTION FOR
EVERY ORGANIZATION
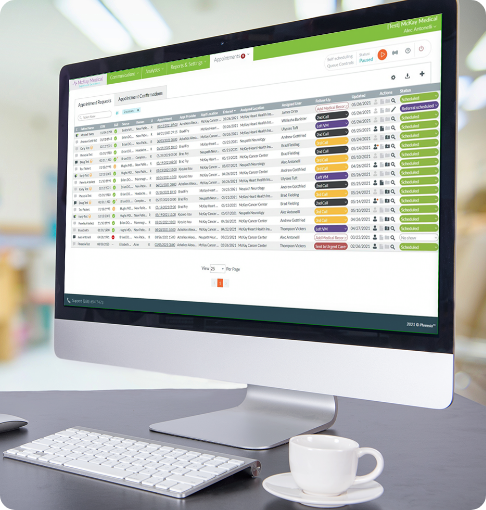
Automate intake, increase collections, see more patients and support patient activation


Rated #1 in Patient Intake Management four years in a row
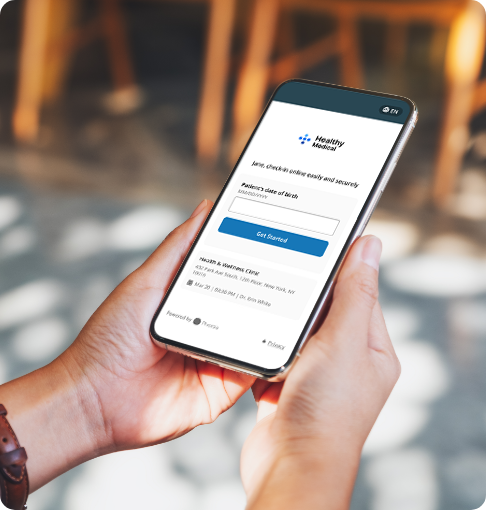
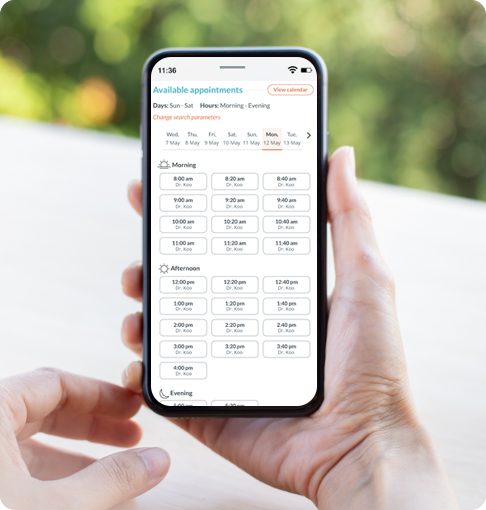
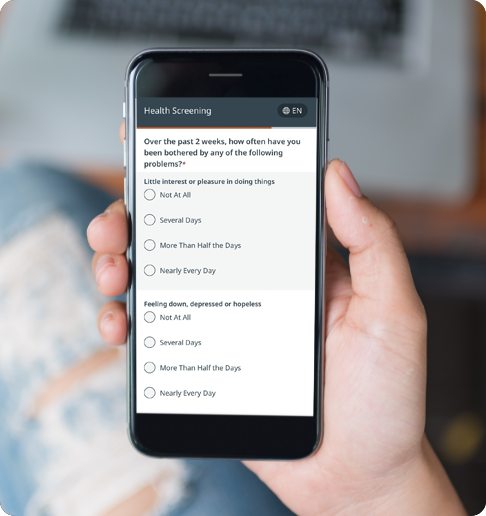
A modern, convenient experience for your patients and staff
Phreesia helps healthcare organizations streamline registration, payments, scheduling, referrals, clinical services and operations. Our customizable platform helps you automate time-consuming tasks and gives your patients an individualized experience at every visit.
Acquire more patients with MediFind, a Phreesia company
Claim your free profile to see why more than 3.5 million providers rely on MediFind
Tailored solutions for every organization
Phreesia partners with healthcare organizations of all sizes. Whether you’re a solo practice, a multispecialty clinic or a busy health system, we offer customizable solutions that help you meet your unique needs and goals.
See who we help:
Fill your administrative staffing gaps
Your staff have more tasks to manage than ever before—and limited resources to manage them. But operating efficiently isn’t about finding more people to do the work. It’s about helping your staff work smarter, not harder.
In just a few short weeks, Phreesia can help you:
- Reduce manual workloads
- Improve efficiency
- Create excellent patient experiences
A customized experience for every patient

Barbara
Phreesia helps healthcare organizations succeed
No matter your size, location or patient demographic, Phreesia can help your organization drive outcomes that matter.
Our bidirectional integrations













Can’t find your PM/EHR? Don’t worry! Phreesia is easily integrated using open standards, including HL7, FHIR, CCD, CSV and more.