Automate Insurance Verification
Stop chasing denials. Start collecting payments.
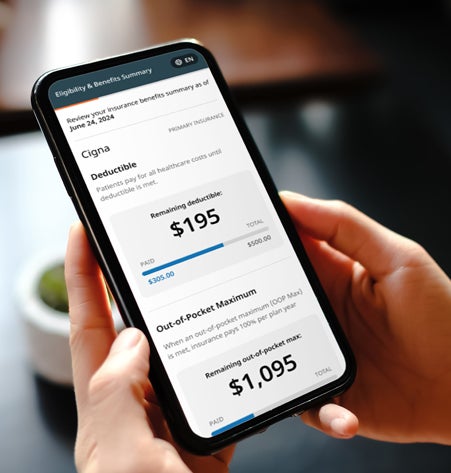
Confirm patient coverage instantly with AI-driven eligibility verification

Automated eligibility checks to reduce claim denials.
Phreesia is the only E&B platform that combines real-time eligibility, AI-driven copay selection and proactive patient workflows—so staff spend less time in payer portals and more time with patients.
What sets Phreesia apart?
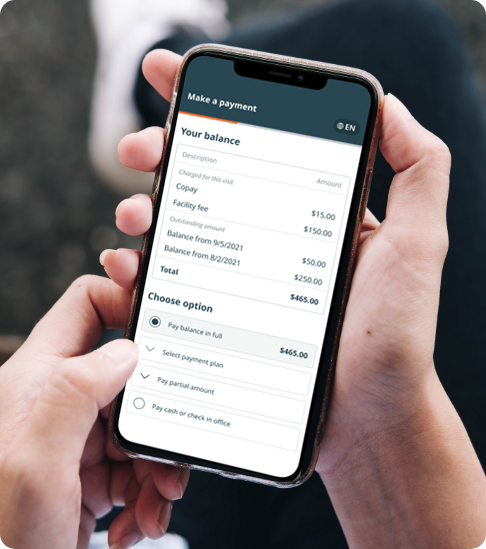
- AI-driven copay selection: Removes guesswork, so patients see and pay the right amount up front
- Smart copay suppression: Suppresses copays when patients have met their out-of-pocket max or when it doesn’t apply to a specific group of patients
- Out-of-network alerting: Flag issues early to prevent claim denials and patient escalations
- Appointment Readiness: Proactively educate patients on their benefits, reducing surprises and delayed care
Ready to reduce denials and get paid faster?
Put AI-enabled eligibility verification to work for your organization.
Short-staffed? We can help.
Staff shortages are not new to healthcare, and many organizations have been dealing with them for years. Luckily, Phreesia is like adding more staff members to your team.
Success stories
No matter your size, location or patient demographic, Phreesia can help your organization drive outcomes that matter.