Effective communication is the bedrock of every patient-provider relationship, but language barriers can jeopardize it. Given that 1 in 5 people speak a language other than English at home, how can healthcare organizations make sure they’re able to connect with every patient?
The answer is simple: Invest in technology that bridges the communication gap.
View our infographic to see the disproportionate risks faced by patients with limited English proficiency—and to learn four benefits of communicating with patients in their preferred language.
Click the image to view the full-sized infographic.
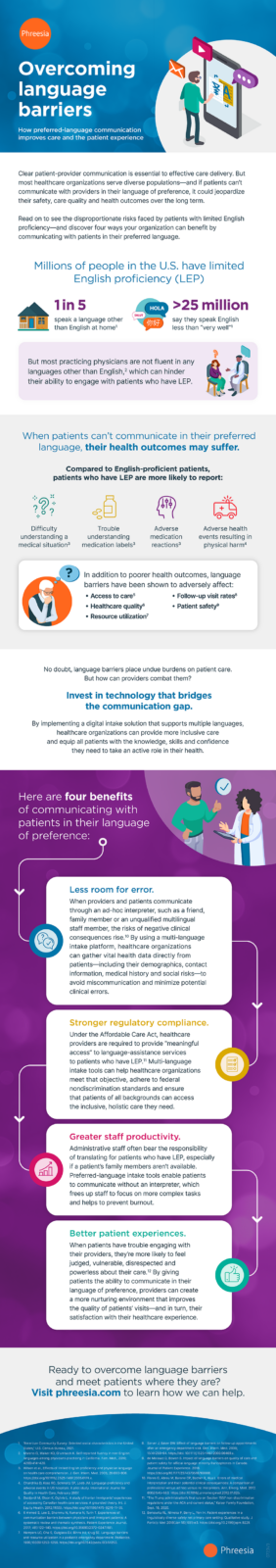
Overcoming language barriers: How preferred-language communication improves care and the patient experience
Clear patient-provider communication is essential to effective care delivery. But most healthcare organizations serve diverse populations—and if patients can’t communicate with providers in their language of preference, it could jeopardize their safety, care quality and health outcomes over the long term.
Read on to see the disproportionate risks faced by patients with limited English proficiency—and discover four ways your organization can benefit by communicating with patients in their preferred language.
Millions of people in the U.S. have limited English proficiency (LEP)
- 1 in 5 speak a language other than English at home1
- >25 million say they speak English less than “very well”1
But most practicing physicians are not fluent in any languages other than English,2 which can hinder their ability to engage with patients who have LEP.
When patients can’t communicate in their preferred language, their health outcomes may suffer.
Compared to English-proficient patients, patients who have LEP are more likely to report:
- Difficulty understanding a medical situation3
- Trouble understanding medication labels3
- Adverse medication reactions3
- Adverse health events resulting in physical harm4
In addition to poorer health outcomes, language barriers have been shown to adversely affect:
- Access to care5
- Healthcare quality6
- Resource utilization7
- Follow-up visit rates8
- Patient safety9
No doubt, language barriers place undue burdens on patient care. But how can providers combat them?
Invest in technology that bridges the communication gap.
By implementing a digital intake solution that supports multiple languages, healthcare organizations can provide more inclusive care and equip all patients with the knowledge, skills and confidence they need to take an active role in their health.
Here are four benefits of communicating with patients in their language of preference:
1. Less room for error.
When providers and patients communicate through an ad-hoc interpreter, such as a friend, family member or an unqualified multilingual staff member, the risks of negative clinical consequences rise.10 By using a multi-language intake platform, healthcare organizations can gather vital health data directly from patients including their demographics, contact information, medical history and social risks—to avoid miscommunication and minimize potential clinical errors.
2. Stronger regulatory compliance.
Under the Affordable Care Act, healthcare providers are required to provide “meaningful access” to language-assistance services to patients who have LEP.11 Multi-language intake tools can help healthcare organizations meet that objective, adhere to federal nondiscrimination standards and ensure that patients of all backgrounds can access the inclusive, holistic care they need.
3. Greater staff productivity.
Administrative staff often bear the responsibility of translating for patients who have LEP, especially if a patient’s family members aren’t available. Preferred-language intake tools enable patients to communicate without an interpreter, freeing up staff to focus on more complex tasks and helping to prevent burnout
4. Better patient experiences.
When patients have trouble engaging with their providers, they’re more likely to feel judged, vulnerable, disrespected and powerless about their care.12 By giving patients the ability to communicate in their language of preference, providers can create a more nurturing environment that improves the quality of patients’ visits and in turn, their satisfaction with their healthcare experience.
Ready to overcome language barriers and meet patients where they are?
Visit phreesia.com to learn how we can help.
Endnotes
1 “American Community Survey: Selected social characteristics in the United States,” U.S. Census Bureau, 2021.
2 Moreno G, Walker KO, Grumbach K. Self-reported fluency in non-English languages among physicians practicing in California. Fam. Med., 2010; 42(6):414–420.
3 Wilson et al., Effects of limited English proficiency and physician language on health care comprehension. J. Gen. Intern. Med. 2005; 20:800–806. https://doi.org/10.1111/j.2525-1497.2005.0174.x.
4 Chandrika D, Koss RG, Schmaltz SP, Loeb JM. Language proficiency and adverse events in US hospitals: A pilot study. International Journal for Quality in Health Care, February 2007.
5 Dastjerdi M, Olson K, Ogilvie L. A study of Iranian immigrants’ experiences of accessing Canadian health care services: A grounded theory. Int. J. Equity Health. 2012;11(55). https://doi.org/10.1186/1475-9276-11-55.
6 Ahmed S, Lee S, Shommu N, Rumana N, Turin T. Experiences of communication barriers between physicians and immigrant patients: A systematic review and thematic synthesis. Patient Experience Journal. 2017; 4(1):122–140. https://doi.org/10.35680/2372-0247.1181.
7 Hampers LC, Cha S, Gutglass DJ, Binns HJ, Krug SE. Language barriers and resource utilization in a pediatric emergency department. Pediatrics. 1999;103(6):1253–1256. https://doi.org/10.1542/peds.103.6.1253.
8 Sarver J, Baker DW. Effect of language barriers on follow-up appointments after an emergency department visit. Gen. Intern. Med. 2000; 15(4):256–64. https://doi: 10.1111/j.1525-1497.2000.06469.x.
9 de Moissac D, Bowen S. Impact of language barriers on quality of care and patient safety for official language minority francophones in Canada. Journal of Patient Experience. 2018. https://doi.org/10.1177/2374373518769008.
10 Flores G, Abreu M, Barone CP, Bacher R, Hua L. Errors of medical interpretation and their potential clinical consequences: A comparison of professional versus ad hoc versus no interpreters. Ann. Emerg. Med. 2012. 60(5):545–553. https://doi:10.1016/j.annemergmed.2012.01.025.
11 “The Trump administration’s final rule on Section 1557 non-discrimination regulations under the ACA and current status,” Kaiser Family Foundation, Sept. 18, 2020.
12 Berkowitz RL, Nimeka P, Berry L, Yen IH. Patient experiences in a linguistically diverse safety net primary care setting: Qualitative study. J Particip Med 2018(Jan 18);10(1):e3. https://doi.org/10.2196/jopm.9229.