Activated patients.
Improved outcomes.
With automated tools for intake, access, payments and more, Phreesia supports patients in taking a more active role in their care and helps you drive outcomes that matter.

Trusted by 3,900+ healthcare organizations nationwide







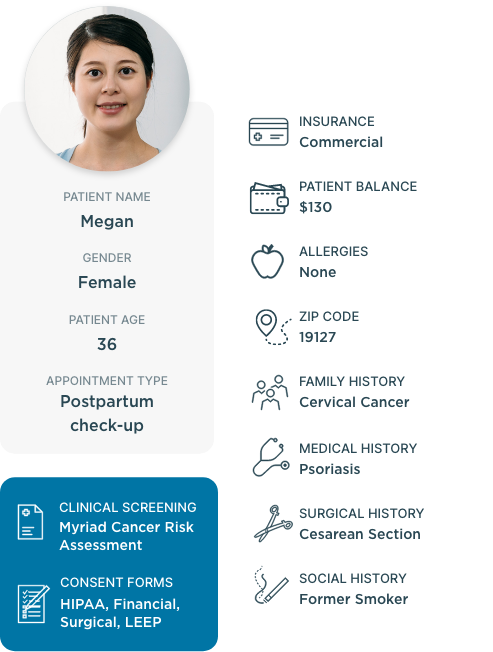
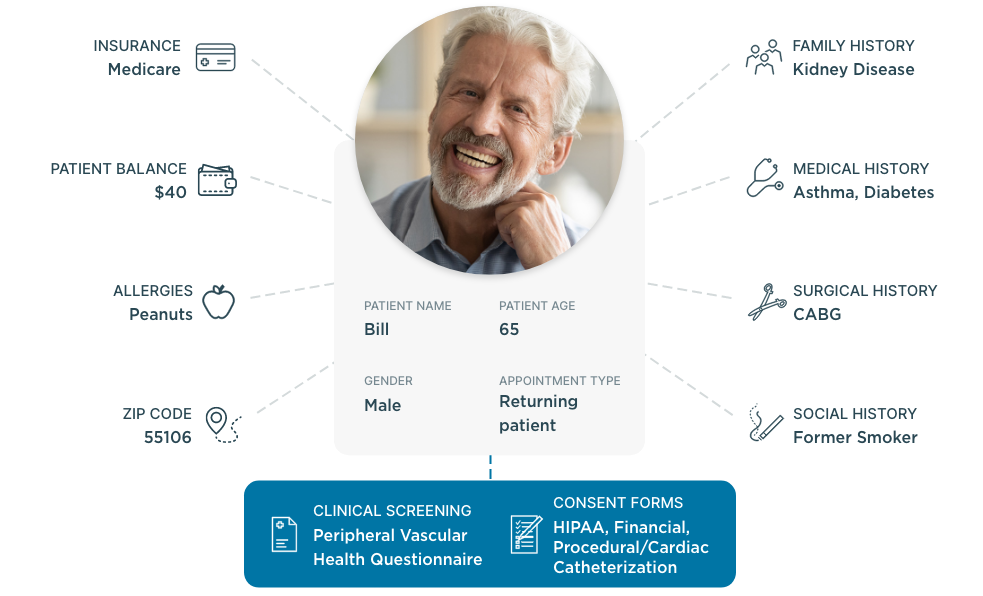
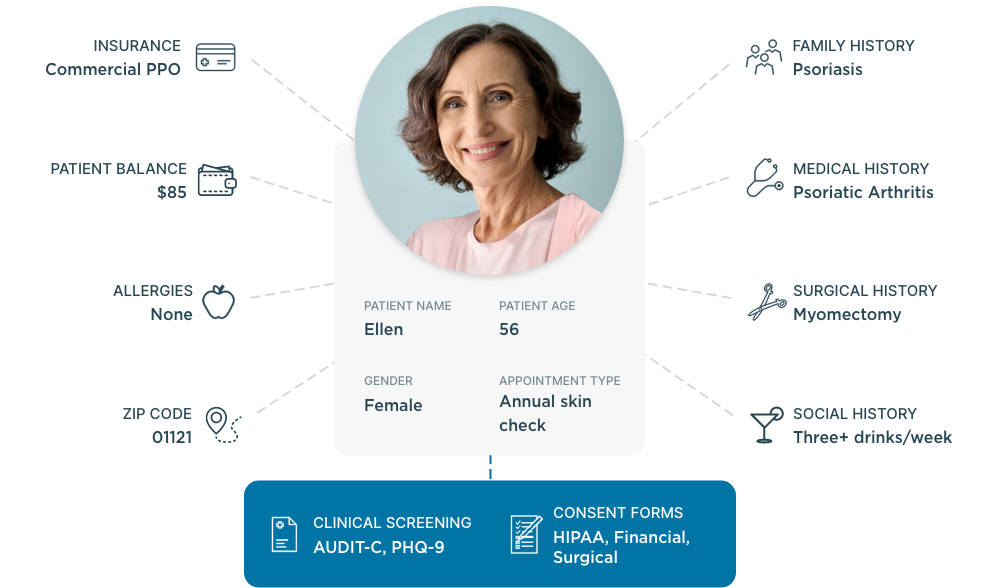
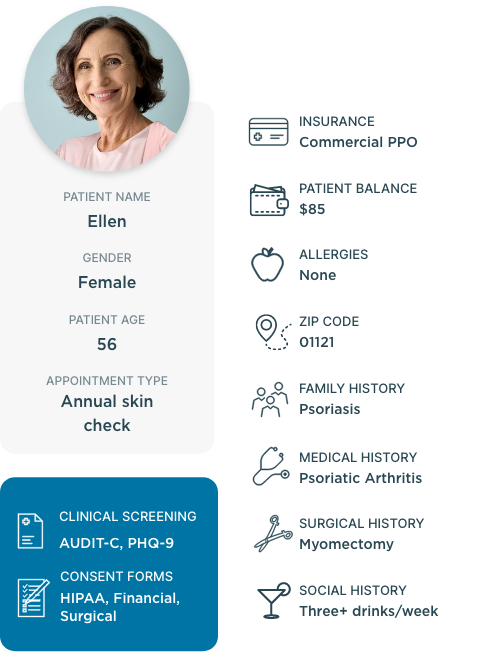
Empower patients to take an active role in their care
When patients feel disengaged and overwhelmed, they’re less likely to understand how to manage their health. But by focusing on patient activation, you can equip patients with the knowledge, skills and confidence they need to actively participate in their care.
Measurable results for your staff and patients
clients would recommend Phreesia to a friend or colleague
of clients say Phreesia creates tangible outcomes for their organization
clients say Phreesia provides high-quality, proactive customer service and support
of patients are satisfied with their experience using Phreesia
Ready to see what Phreesia could do for you? Use our calculators >
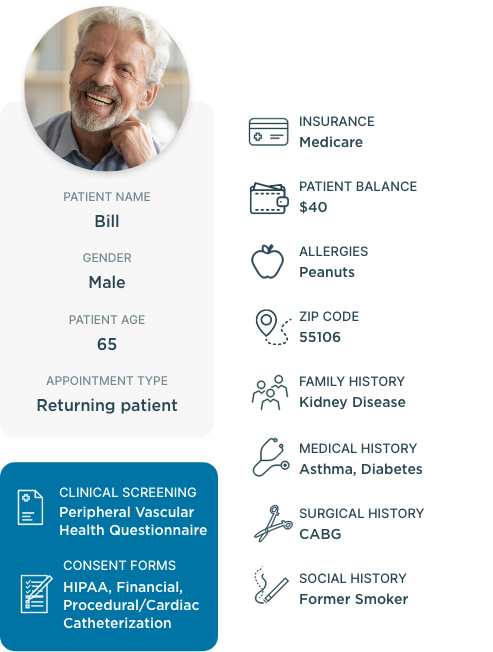
Fill your administrative staffing gaps
Between appointments, registration, insurance verification and patient outreach, your organization has lots of tasks to manage—and limited resources to manage them. But operating efficiently isn’t about finding more people to do the work. It’s about helping your staff work smarter, not harder.
Browse our resources
Keep tabs on our latest announcements, media coverage, expert insights and more.
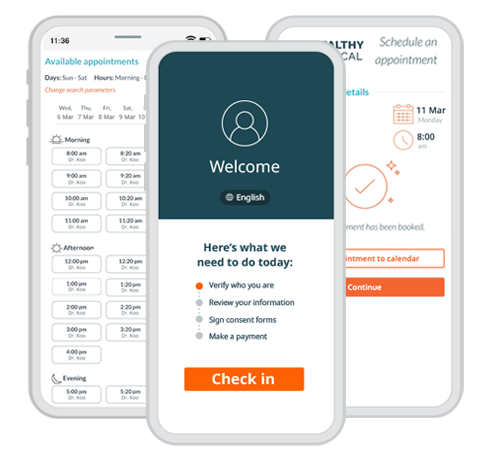
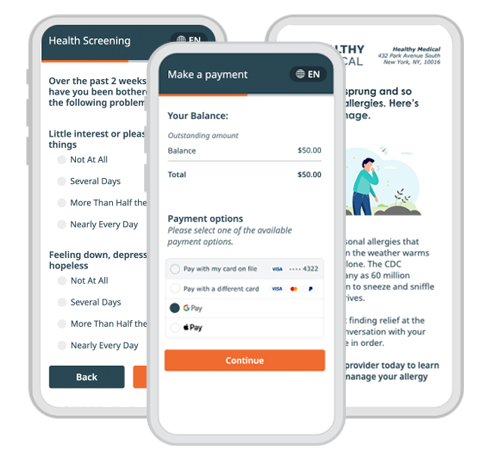
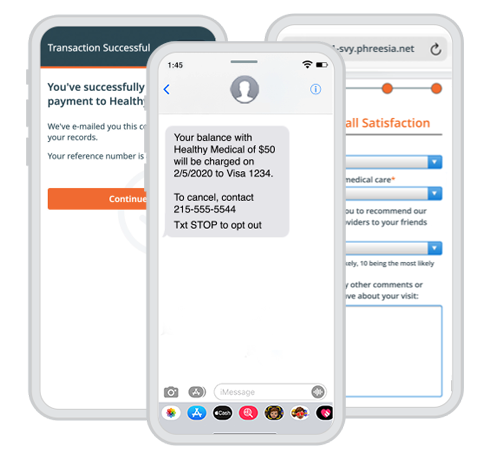
Patient engagement journey
Support your organization’s digital front-door strategy and engage patients at every step of their healthcare
journey with native applications and a library of APIs.
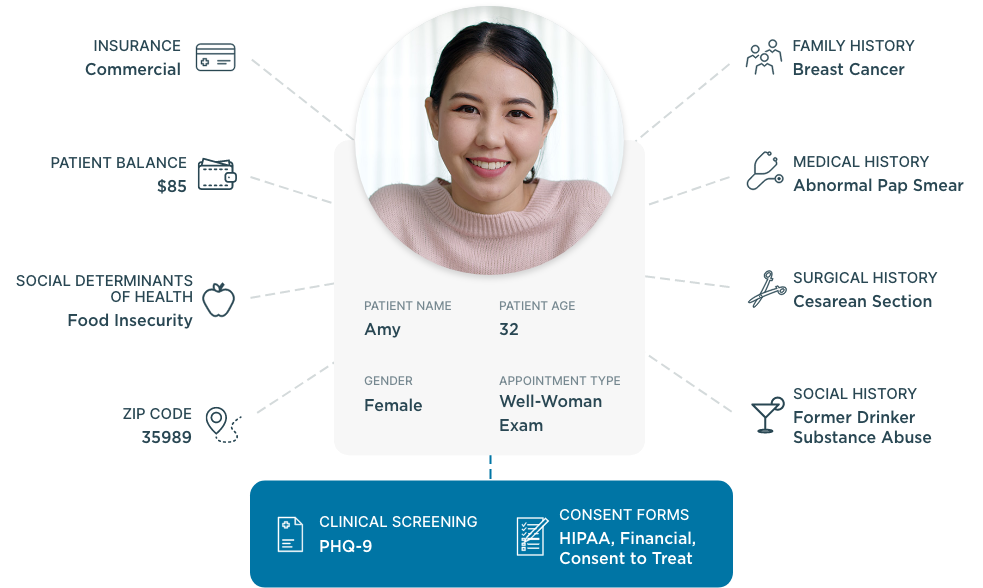
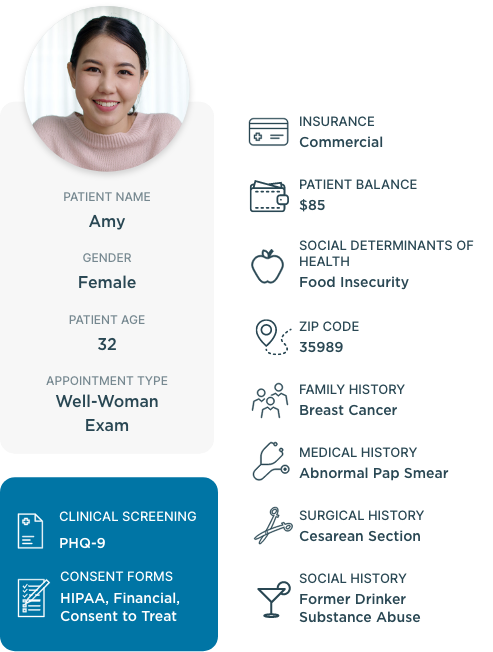
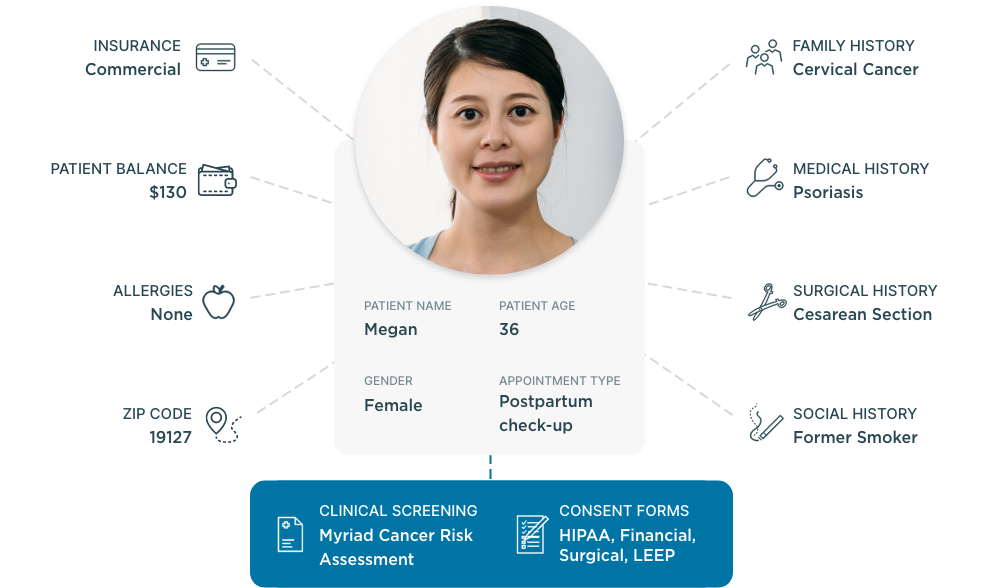
Select your organization type to see a tailored solution
What our clients say about us
Our bidirectional integrations













Can’t find your PM/EHR? Don’t worry! Phreesia is easily integrated using open standards, including HL7, FHIR, CCD, CSV and more.