As the Merit-based Incentive Payment System (MIPS) enters its sixth year of existence, the Centers for Medicare and Medicaid Services (CMS) has made a number of changes to the program as it continues to move toward a more holistic, value-based framework.
In Year 6, CMS has designed MIPS to better advance health equity, address social determinants of health, and ensure scoring is fair for small practices, which have historically borne the brunt of negative payment adjustments.
The following infographic captures important takeaways for MIPS this year, including changes to the program for 2022, eligibility criteria, a breakdown of how scores are calculated and what’s at stake for the future. You also will see that data for a variety of MIPS measures, including cervical cancer screening, fall risk assessment, documentation of current medications and many others, can be automatically captured during the intake process.
Click the image to view the full-sized infographic
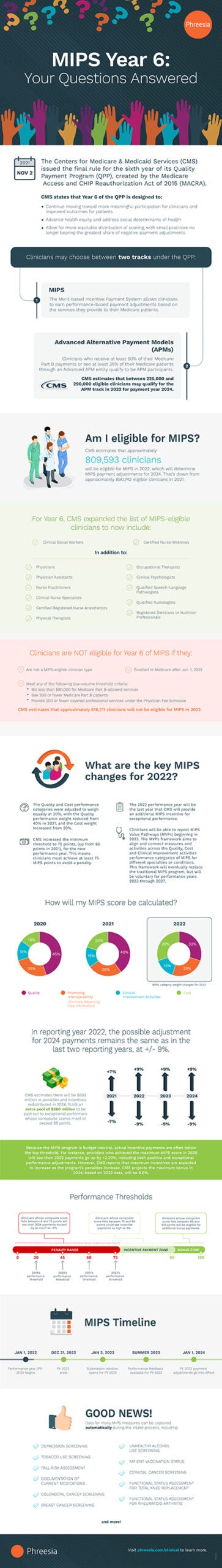
MIPS Year 6: Your Questions Answered
The Centers for Medicare & Medicaid Services (CMS) issued the final rule for the sixth year of its Quality Payment Program (QPP), created by the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA).
CMS states that Year 6 the QPP is designed to:
- Continue moving toward more meaningful participation for clinicians and improved outcomes for patients
- Advance health equity and address social determinants of health
- Allow for more equitable distribution of scoring, with small practices no longer bearing greatest share of negative payment adjustments
Clinicians may choose between two tracks under the QPP:
- MIPS: The Merit-based Incentive Payment System allows clinicians to earn performance-based payment adjustments based on the services they provide to their Medicare patients.
- Advanced Alternative Payment Models (APMs): Clinicians who receive at least 50% of their Medicare Part B payments or see at least 35% of their Medicare patients through an Advanced APM entity qualify to be APM participants.
CMS estimates that between 225,000 and 290,000 eligible clinicians may qualify for the APM track in 2022 for payment year 2024.
AM I ELIGIBLE FOR MIPS?
CMS estimates that approximately 809,593 clinicians will be eligible for MIPS in 2022, which will determine MIPS payment adjustments for 2024. That’s down from approximately 890,742 eligible clinicians in 2021.
For Year 6, CMS expanded the list of MIPS-eligible clinicians to now include:
- Clinical Social Workers
- Certified Nurse-Midwives
In addition to:
- Physicians
- Physician Assistants
- Nurse Practitioners
- Clinical Nurse Specialists
- Certified Registered Nurse Anesthetists
- Physical Therapists
- Occupational Therapists
- Clinical Psychologists
- Qualified Speech-Language Pathologists
- Qualified Audiologists
- Registered Dieticians or Nutrition Professionals
Clinicians are NOT eligible for Year 6 of MIPS if they:
- Are not a MIPS-eligible clinician type
- Enrolled in Medicare after Jan. 1, 2022
- Meet any of the following low-volume threshold criteria:
- Bill less than $90,000 for Medicare Part B-allowed services
- See 200 or fewer Medicare Part B patients
- Provide 200 or fewer covered professional services under the Physician Fee Schedule
CMS estimates that approximately 816,211 clinicians will not be eligible for MIPS in 2022.
WHAT ARE THE KEY MIPS CHANGES FOR 2022?
- The Quality and Cost performance category weights were were adjusted to weigh equally at 30%, with the Quality performance weight reduced from 40% in 2021, and the Cost weight increased from 20%.
- CMS increased the minimum threshold to 75 points, (up from 60 points in 2021), for the new performance year. This means clinicians must achieve at least 75 MIPS points to avoid a penalty.
- The 2022 performance year will be the last year that CMS will provide an additional MIPS incentive for exceptional performance.
- Clinicians will be able to report MIPS Value Pathways (MVPs) beginning in 2023. The MVPs framework aims to align and connect measures and activities across the Quality, Cost and Clinical Improvement activities performance categories of MIPS for different specialties or conditions. This framework will eventually replace the traditional MIPS program, but will be voluntary for performance years 2023 through 2027.
HOW WILL MY MIPS SCORE BE CALCULATED?
2020
- Quality: 45%
- Promoting Interoperability: 25%
- Improvement Activities: 15%
- Cost: 15%
2021
- Quality: 40%
- Promoting Interoperability: 25%
- Improvement Activities: 15%
- Cost: 20%
2022
- Quality: 30%
- Promoting Interoperability: 25%
- Clinical Improvement Activities: 15%
- Cost: 30%
In reporting year 2022, the possible adjustment for 2024 payments remains the same as in the last two reporting years, at +/- 9%.
CMS estimates there will be $603 million in penalties and incentives redistributed in 2024, PLUS an extra pool of $360 million to be paid out to exceptional performers whose composite scores meet or exceed 89 points.
- 2021: +/- 7%
- 2022: +/- 9%
- 2023: +/- 9%
- 2024: +/- 9%
Because the MIPS program is budget-neutral, actual incentive payments are ofen below the top threshold. For instance, providers who achieved the maximum MIPS score in 2020 will see their 2022 payments go up by +2.20%, including both positive and exceptional performance adjustments. However, CMS reports that maximum incentives are expected to increase as the program’s penalties increase. CMS projects the maximum bonus in 2024, based on 2022 data, will be 6.6%.
Performance Thresholds
Clinicians whose composite score falls between 0 and 75 points will see their 2024 payments docked by as much as -9%.
Clinicians whose composite score falls between 75 and 89 points could see incentive payments as high as 9%.
Clinicians whose composite score falls between 89 and 100 points will be eligible for additional bonus payments.
- 2019 performance threshold: 30 points
- 2020 performance threshold: 45 points
- 2021 performance threshold: 60 points
- 2022 performance threshold: 75 points
MIPS TIMELINE
JAN 1, 2022: Performance year (PY) 2022 begins
DEC 31, 2022: PY 2022 ends
JAN 2, 2023: Submission window opens for PY 2022
SUMMER 2023: Performance feedback available for PY 2022
JAN 1, 2024: PY 2022 payment adjustments go into effect
GOOD NEWS!
Data for many MIPS measures can be captured automatically during the intake process, including:
- Depression Screening
- Tobacco Use Screening
- Fall Risk Assessment
- Documentation of Current Medications
- Colorectal Cancer Screening
- Breast Cancer Screening
- Unhealthy Alcohol Use Screening
- Patient Vaccination Status
- Cervical Cancer Screening
- Functional Status Assessment for Total Knee Replacement
- Functional Status Assessment for Rheumatoid Arthritis
and more!
Visit phreesia.com/clinical to learn more.