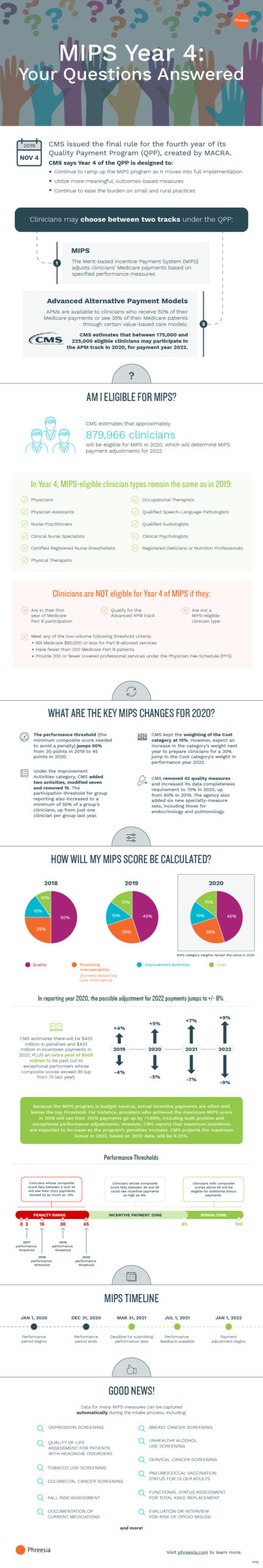
CMS made a number of significant changes to the Merit-Based Incentive Payment System (MIPS) for the program’s fourth year. Now’s the time to ensure you’re familiar with those changes so your practice can avoid a penalty—and hopefully receive a payment bump—in 2022.
Check out our latest infographic for important takeaways from the fourth year of MIPS—including key changes to the program for 2020, information on how scores are calculated, who is eligible and what’s at stake—and to learn how data for many MIPS measures, such as depression screening, fall risk and colorectal cancer screening, can be captured automatically during the intake process.
Click the image to view the full-sized infographic
MIPS Year 4: Your Questions Answered
CMS issued the final rule for the fourth year of its Quality Payment Program (QPP), created by MACRA.
CMS says Year 4 of the QPP is designed to:
- Continue to ramp up the MIPS program as it moves into full implementation
- Utilize more meaningful, outcomes-based measures
- Continue to ease the burden on small and rural practices
Clinicians may choose between two tracks under the QPP:
- MIPS: The Merit-based Incentive Payment System (MIPS) adjusts clinicians’ Medicare payments based on specified performance measures.
- Advanced Alternative Payment Models: APMs are available to clinicians who receive 50% of their Medicare payments or see 35% of their Medicare patients through certain value-based care models.CMS estimates that between 175,000 and 225,000 eligible clinicians may participate in the APM track in 2020, for payment year 2022.
AM I ELIGIBLE FOR MIPS?
CMS estimates that approximately 879,966 clinicians will be eligible for MIPS in 2020, which will determine MIPS payment adjustments for 2022.
In Year 4, MIPS-eligible clinician types remain the same as in 2019:
- Physicians
- Physician Assistants
- Nurse Practitioners
- Clinical Nurse Specialists
- Certified Registered Nurse Anesthetists
- Physical Therapists
- Occupational Therapists
- Qualified Speech-Language Pathologists
- Qualified Audiologists
- Clinical Psychologists
- Registered Dieticians or Nutrition Professionals
Clinicians are NOT eligible for Year 4 of MIPS if they:
- Are in their first year of Medicare Part B participation
- Qualify for the Advanced APM track
- Are not a MIPS-eligible clinician type
- Meet any of the low-volume following threshold criteria:
- Bill Medicare $90,000 or less for Part B-allowed services
- Have fewer than 200 Medicare Part B patients
- Provide 200 or fewer covered professional services under the Physician Fee Schedule (PFS)
WHAT ARE THE KEY MIPS CHANGES FOR 2020?
- The performance threshold (the minimum composite score needed to avoid a penalty) jumps 50% from 30 points in 2019 to 45 points in 2020.
- Under the Improvement Activities category, CMS added two activities, modified seven and removed 15. The participation threshold for group reporting also increased to a minimum of 50% of a group’s clinicians, up from just one clinician per group last year.
- CMS kept the weighting of the Cost category at 15%. However, expect an increase in the category’s weight next year to prepare clinicians for a 30% jump in the Cost category’s weight in performance year 2022.
- CMS removed 42 quality measures and increased its data completeness requirement to 70% in 2020, up from 60% in 2019. The agency also added six new specialty-measure sets, including those for endocrinology and pulmonology.
HOW WILL MY MIPS SCORE BE CALCULATED?
- 2018
- Quality: 50%
- Promoting Interoperability
(formerly Advancing Care Information): 25% - Improvement Activities: 15%
- Cost: 10%
- 2019
- Quality: 45%
- Promoting Interoperability
(formerly Advancing Care Information): 25% - Improvement Activities: 15%
- Cost: 15%
- 2020: MIPS category weights remain the same in 2020.
- Quality: 45%
- Promoting Interoperability
(formerly Advancing Care Information): 25% - Improvement Activities: 15%
- Cost: 15%
In reporting year 2020, the possible adjustment for 2022 payments jumps to +/- 9%.
CMS estimates there will be $433 million in penalties and $433 million in incentives payments in 2022, PLUS an extra pool of $500 million to be paid out to exceptional performers whose composite scores exceed 85 (up from 75 last year).
- 2019: +/- 4%
- 2020: +/- 5%
- 2021: +/- 7%
- 2022: +/- 9%
Because the MIPS program is budget-neutral, actual incentive payments are often well below the top threshold. For instance, providers who achieved the maximum MIPS score in 2018 will see their 2020 payments go up by +1.68%, including both positive and exceptional performance adjustments. However, CMS reports that maximum incentives are expected to increase as the program’s penalties increase. CMS projects the maximum bonus in 2022, based on 2020 data, will be 6.25%.
Performance Thresholds
- Clinicians whose composite score falls between 0 and 45 will see their 2022 payments docked by as much as -9%.
- 2017 performance threshold: 3
- 2018 performance threshold: 15
- 2019 performance threshold: 30
- 2020 performance threshold: 45
- Clinicians whose composite score falls between 45 and 85 could see incentive payments as high as 9%.
- Clinicians with composite scores above 85 will be eligible for additional bonus payments.
MIPS TIMELINE
- JAN 1, 2020: Performance period begins
- DEC 31, 2020: Performance period ends
- MAR 31, 2021: Deadline for submitting performance data
- JUL 1, 2021: Performance feedback available
- JAN 1, 2022: Payment adjustment begins
GOOD NEWS!
Data for many MIPS measures can be captured automatically during the intake process, including:
- DEPRESSION SCREENING
- QUALITY OF LIFE ASSESSMENT FOR PATIENTS WITH HEADACHE DISORDERS
- TOBACCO USE SCREENING
- COLORECTAL CANCER SCREENING
- FALL RISK ASSESSMENT
- DOCUMENTATION OF CURRENT MEDICATIONS
- BREAST CANCER SCREENING
- UNHEALTHY ALCOHOL USE SCREENING
- CERVICAL CANCER SCREENING
- PNEUMOCOCCAL VACCINATION STATUS FOR OLDER ADULTS
- FUNCTIONAL STATUS ASSESSMENT FOR TOTAL KNEE REPLACEMENT
- EVALUATION OR INTERVIEW FOR RISK OF OPIOID MISUSE
- AND MORE!